Additive Manufactured Fixation Plates Match Stiffness and Shape of Patient’s Jaw Bone
Research shows that NiTi fixation plates manufactured with controlled porosity using SLM can be matched to the stiffness of a patient’s lower jaw bone as well as its shape.
Share
Fixation plates are critical following reconstructive surgery, as they help bear strain, guide healing and encourage the vascularization of bone graft. But once the bone has healed, a plate that is too stiff increases the risk of abnormal stress distribution. One possible outcome is reduced stress, called stress shielding, between the grafted and host bone. Stress-shielded bone may resorb, leading to implant failure.
The most commonly used material for skeletal fixation devices is Ti-6Al-4V. Traditionally, fixation plates are made to standard sizes from this material, and then bent in the operating room to fit the patient’s anatomy. The high stiffness of Ti-6Al-4V relative to cortical bone can make these implants more prone to fail.
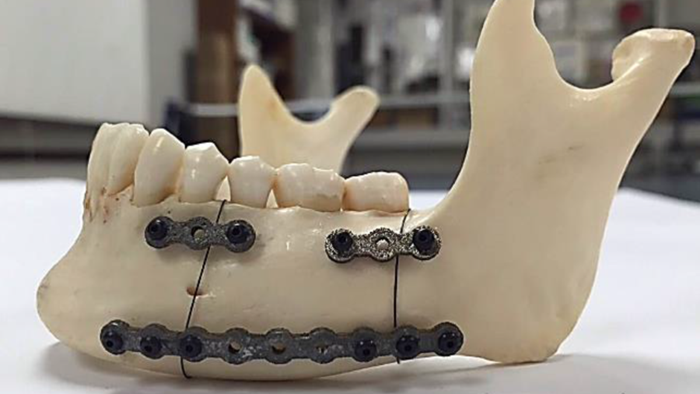
In a study published by open access journal Bioengineering, a team of researchers 3D printed fixation plates for mandible, or lower jaw, reconstruction surgery using a different material, NiTi. Their goal was to achieve a more natural stress distribution and increase pressure at the graft/host interface to avoid stress shielding. Using additive manufacturing technology, the team developed porous NiTi fixation plates that can be customized to match the patient’s mandible shape and bone stiffness.
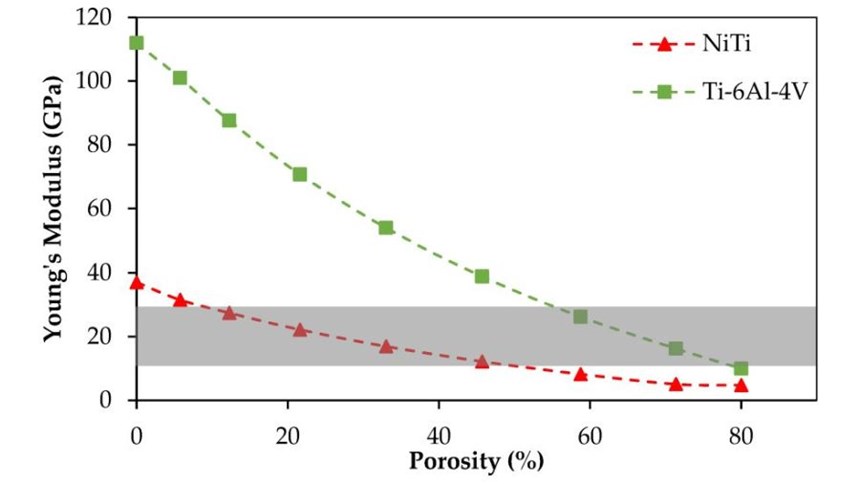
Initial dense samples made with NiTi using selective laser melting (SLM) had a Young’s modulus of 37 GPa. According to research cited in the study, cortical bone in the adult mandible ranges from 10 to 31.2 GPa. Using CT scanning, the team determined that the cadaver mandible used in the study had a Young’s modulus of 12 GPa.
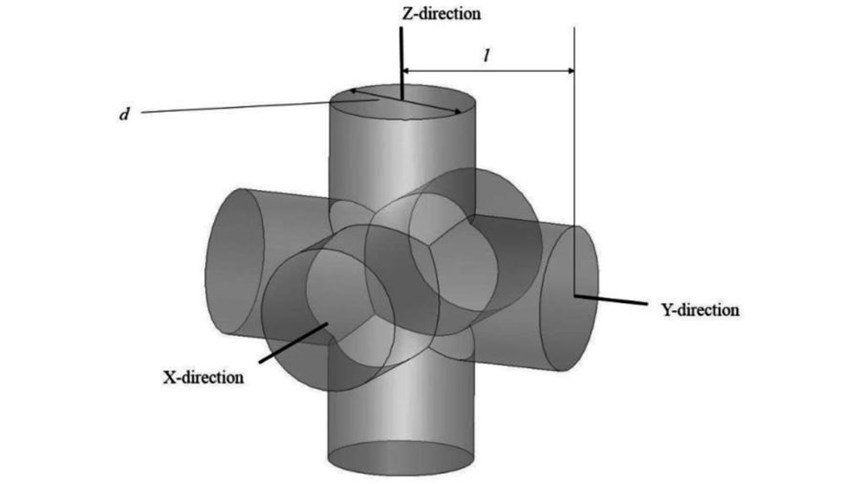
To reduce the stiffness of the NiTi material and match it to the sample mandible, the researchers introduced porosity using identical unit cells (see the second slide, above). Each of these cells is composed of three intersecting cylinders all with the same diameter. The level of porosity can be tuned by changing the diameter of the cylinders.
Researchers calculated that 45.7 percent porosity in the first fixation plate would be necessary to match the bone’s 12 GPa Young’s modulus, which meant a diameter of 1 mm for the pore unit cells. The same stiffness could also be achieved with SLM and Ti-6Al-4V; however, this would require a much higher porosity of 78.3 percent, which can cause complications during manufacturing. (See the third slide, above.)
The fixations were produced via SLM on a Phenix PXM system. Following printing, the plates underwent heat treatment procedures including solution annealing and aging to induce superelasticity. Then, the NiTi plates and standard Ti-6Al-4V fixation plates were simulated in three loading scenarios to study the stress distribution.
The researchers concluded that the porous NiTi fixations were superior to Ti-6Al-4V fixations because the material enabled decreasing the stiffness of the fixation plates to match the stiffness of the surrounding bone, minimizing the probability of stress shielding, at a lower percentage porosity. Additionally, fabricating the NiTi plates with selective laser melting ensured a custom fit for the patient and could reduce operating room time.
Related Content
-
Zeda AM Production Plant in Ohio Now Open — Thoughts on the New Facility
73,000-square-foot metal powder bed fusion plant includes extensive machining capability plus separate operational models for serving medical versus other businesses.
-
Overcoming Challenges with 3D Printing Nitinol (and Other Oxygen-Sensitive Alloys) Through Atmospheric Control
3D printed nitinol has potential applications in dental, medical and more but oxygen pickup can make this material challenging to process. Linde shares how atmospheric monitoring and the use of special gas mixtures can help maintain the correct atmosphere for printing this shape alloy and other metals.
-
8 Cool Parts From Formnext 2023: The Cool Parts Show #65
New additive manufacturing technologies on display at Formnext were in many cases producing notable end-use components. Here are some of the coolest parts we found at this year’s show.
.jpg;width=70;height=70;mode=crop)