Additive Manufactured Fixation Plates Match Stiffness and Shape of Patient’s Jaw Bone
Research shows that NiTi fixation plates manufactured with controlled porosity using SLM can be matched to the stiffness of a patient’s lower jaw bone as well as its shape.
Fixation plates are critical following reconstructive surgery, as they help bear strain, guide healing and encourage the vascularization of bone graft. But once the bone has healed, a plate that is too stiff increases the risk of abnormal stress distribution. One possible outcome is reduced stress, called stress shielding, between the grafted and host bone. Stress-shielded bone may resorb, leading to implant failure.
The most commonly used material for skeletal fixation devices is Ti-6Al-4V. Traditionally, fixation plates are made to standard sizes from this material, and then bent in the operating room to fit the patient’s anatomy. The high stiffness of Ti-6Al-4V relative to cortical bone can make these implants more prone to fail.
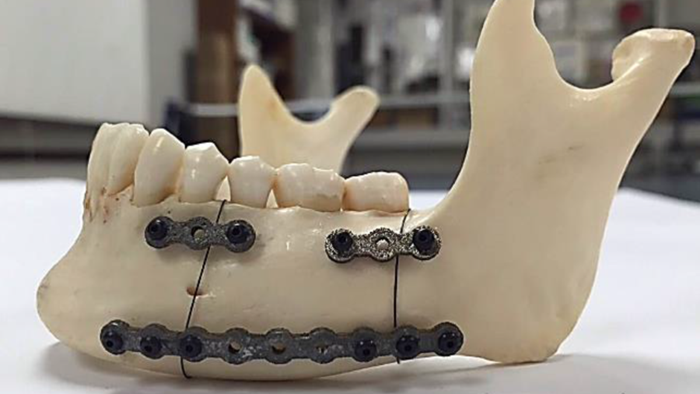
In a study published by open access journal Bioengineering, a team of researchers 3D printed fixation plates for mandible, or lower jaw, reconstruction surgery using a different material, NiTi. Their goal was to achieve a more natural stress distribution and increase pressure at the graft/host interface to avoid stress shielding. Using additive manufacturing technology, the team developed porous NiTi fixation plates that can be customized to match the patient’s mandible shape and bone stiffness.
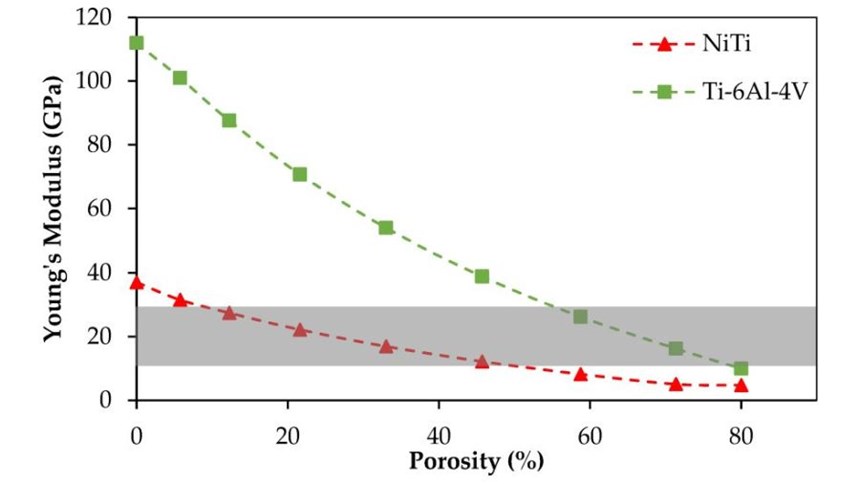
Initial dense samples made with NiTi using selective laser melting (SLM) had a Young’s modulus of 37 GPa. According to research cited in the study, cortical bone in the adult mandible ranges from 10 to 31.2 GPa. Using CT scanning, the team determined that the cadaver mandible used in the study had a Young’s modulus of 12 GPa.
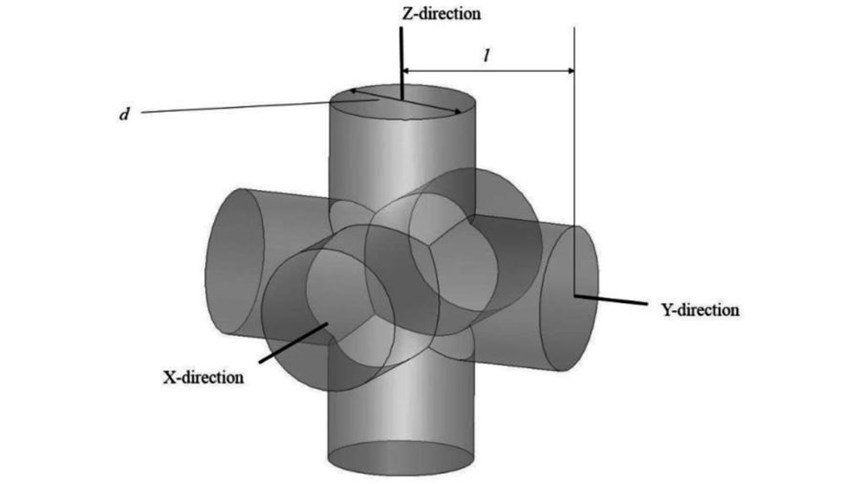
To reduce the stiffness of the NiTi material and match it to the sample mandible, the researchers introduced porosity using identical unit cells (see the second slide, above). Each of these cells is composed of three intersecting cylinders all with the same diameter. The level of porosity can be tuned by changing the diameter of the cylinders.
Researchers calculated that 45.7 percent porosity in the first fixation plate would be necessary to match the bone’s 12 GPa Young’s modulus, which meant a diameter of 1 mm for the pore unit cells. The same stiffness could also be achieved with SLM and Ti-6Al-4V; however, this would require a much higher porosity of 78.3 percent, which can cause complications during manufacturing. (See the third slide, above.)
The fixations were produced via SLM on a Phenix PXM system. Following printing, the plates underwent heat treatment procedures including solution annealing and aging to induce superelasticity. Then, the NiTi plates and standard Ti-6Al-4V fixation plates were simulated in three loading scenarios to study the stress distribution.
The researchers concluded that the porous NiTi fixations were superior to Ti-6Al-4V fixations because the material enabled decreasing the stiffness of the fixation plates to match the stiffness of the surrounding bone, minimizing the probability of stress shielding, at a lower percentage porosity. Additionally, fabricating the NiTi plates with selective laser melting ensured a custom fit for the patient and could reduce operating room time.
Related Content
-
3D Printed Spine Implants Made From PEEK Now in Production
Medical device manufacturer Curiteva is producing two families of spinal implants using a proprietary process for 3D printing porous polyether ether ketone (PEEK).
-
Cranial Implant 3D Printed From Hydroxyapatite Ceramic: The Cool Parts Show #76
Cranial implants are typically made from titanium or PEEK; in this episode of The Cool Parts Show, we look at how implants made from a bioceramic can improve osseointegration and healing.
-
Micro Robot Gripper 3D Printed All at Once, No Assembly Required: The Cool Parts Show #59
Fine control over laser powder bed fusion achieves precise spacing between adjoining moving surfaces. The Cool Parts Show looks at micro 3D printing of metal for moving components made in one piece.
.jpg;width=70;height=70;mode=crop)